Andamios porosos para ingeniería de tejidos óseos: características geométricas, requerimientos de uso, y materiales y métodos de manufactura aditiva
Palabras clave:
Ingeniería de tejidos óseos, Material celular, Diseño de soportes, Manufactura aditivaContenido principal del artículo
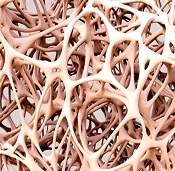
Los materiales con una estructura porosa interna que reemplazan hueso dañado y sirven como andamios para pro-cesos regenerativos son una herramienta fundamental en la ingeniería de tejidos óseos. En los últimos años, se ha investigado sobre la geometría interna que deben tener los andamios de modo que respondan a requerimientos específicos. El objetivo de esta revisión es mostrar los biomateriales y métodos de manufactura aditiva que se usan en la fabricación de andamios, las principales características geométricas de las celdas que conforman los materiales celulares, las formas que estas celdas se distribuyen en el espacio entre otros. Para la revisión sistemática se consultó la base de datos Google Scholar. Para esto se usaron los términos en inglés: bone tissue engineering scaffold geometric design. Los criterios de inclusión fueron que los documentos estuvieran en idioma inglés y estuvieran publicados de 2018 en adelante. Se revisaron los primeros 200 resultados y se priorizaron aquellos que eran artículos de revisión. Se destacó la importancia del tamaño de poro y porcentaje de porosidad como las propiedades geométricas que más influyen en las propiedades mecánicas, biológicas y de permeabilidad del andamio. Se muestra como la investigación actual tiende hacia biomateriales degradables que puedan generar una respuesta en el tejido que crece sobre ellos y el diseño de estructuras en donde la búsqueda de una propiedad requerida guía el diseño del andamio mediante métodos procedimentales o de optimización lo que supone un cambio frente al estudio de una o más celdas para establecer si sus propiedades se ajustaban a lo requerido.
Abbasi N, Hamlet S, Love RM, Nguyen NT. Porous scaffolds for bone regeneration. J Sci Adv Mater Devices [Internet]. 2020;5(1):1–9. Available from: https://doi.org/10.1016/j.jsamd.2020.01.007 DOI: https://doi.org/10.1016/j.jsamd.2020.01.007
Marco F, Galán-Olleros M, Mora-Fernández J. Hip fracture: A 21st century socio-sanitary epidemic in the first world. An RANM. 2019 Jan 2;135(03):203–10. DOI: https://doi.org/10.32440/ar.2018.135.03.rev01
Kanwar S, Vijayavenkataraman S. Design of 3D printed scaffolds for bone tissue engineering: A review. Bioprinting. 2021 Dec 1;24:e00167. DOI: https://doi.org/10.1016/j.bprint.2021.e00167
Bahraminasab M. Challenges on optimization of 3D-printed bone scaffolds. Biomed Eng Online [Internet]. 2020 Sep 3 [cited 2022 May 6];19(1):1–33. Available from: https://biomedical-engineering-online.biomedcentral.com/articles/10.1186/s12938-020-00810-2 DOI: https://doi.org/10.1186/s12938-020-00810-2
Wu T, Yu S, Chen D, Wang Y. Bionic design, materials and performance of bone tissue scaffolds. Materials (Basel). 2017;10(10). DOI: https://doi.org/10.3390/ma10101187
Grand View Research. Bone Grafts And Substitutes Market Size, Share & Trends Analysis Report By Material Type (Allograft, Synthetic), By Application (Spinal Fusion, Foot & Ankle, Joint Reconstruction), By Region, And Segment Forecasts, 2022 - 2030 [Internet]. Market analysis report. 2022. Available from: https://www.grandviewresearch.com/industry-analysis/bone-grafts-substitutes-market
Kalsi S, Singh J, Sehgal SS, Sharma NK. Biomaterials for tissue engineered bone Scaffolds : A review. Mater Today Proc. 2021;2214–7853.
Li Z, Du T, Ruan C, Niu X. Bioinspired mineralized collagen scaffolds for bone tissue engineering. Bioact Mater. 2021;6(5):1491–511. DOI: https://doi.org/10.1016/j.bioactmat.2020.11.004
Hu C, Ashok D, Nisbet DR, Gautam V. Bioinspired surface modification of orthopedic implants for bone tissue engineering. Biomaterials. 2019;219(July):119366. DOI: https://doi.org/10.1016/j.biomaterials.2019.119366
Zhu G, Zhang T, Chen M, Yao K, Huang X, Zhang B, et al. Bone physiological microenvironment and healing mechanism: Basis for future bone-tissue engineering scaffolds. Bioact Mater. 2021;6(11):4110–40. DOI: https://doi.org/10.1016/j.bioactmat.2021.03.043
Elise F. Morgan LCG. Chapter 2 - The bone organ system: form and function. Marcus Feldman’s Osteoporos (Fifth Ed Acad Press. 2021;15–35. DOI: https://doi.org/10.1016/B978-0-12-813073-5.00002-2
Ott SM. Cortical or Trabecular Bone: What’s the Difference? Am J Nephrol. 2018;47(6):373–5. DOI: https://doi.org/10.1159/000489672
Christy PN, Basha SK, Kumari VS, Bashir AKH, Maaza M, Kaviyarasu K, et al. Biopolymeric nanocomposite scaffolds for bone tissue engineering applications – A review. J Drug Deliv Sci Technol. 2020;55(September 2019). DOI: https://doi.org/10.1016/j.jddst.2019.101452
Vammi S, Bukyya JL, CK AA, Tejasvi MLA, Pokala A, HP C, et al. Genetic Disorders of Bone or Osteodystrophies of Jaws—A Review. Glob Med Genet. 2021;08(02):41–50. DOI: https://doi.org/10.1055/s-0041-1724105
Shirzad M, Zolfagharian A, Matbouei A, Bodaghi M. Design, evaluation, and optimization of 3D printed truss scaffolds for bone tissue engineering. J Mech Behav Biomed Mater. 2021;120(March):104594. DOI: https://doi.org/10.1016/j.jmbbm.2021.104594
Eltom A, Zhong G, Muhammad A. Scaffold Techniques and Designs in Tissue Engineering Functions and Purposes: A Review. Adv Mater Sci Eng. 2019;2019. DOI: https://doi.org/10.1155/2019/3429527
Baptista R, Guedes M. Morphological and mechanical characterization of 3D printed PLA scaffolds with controlled porosity for trabecular bone tissue replacement. Mater Sci Eng C. 2021;118(May 2020). DOI: https://doi.org/10.1016/j.msec.2020.111528
Qu H. Additive manufacturing for bone tissue engineering scaffolds. Mater Today Commun. 2020 Sep 1;24:101024. DOI: https://doi.org/10.1016/j.mtcomm.2020.101024
Giannitelli SM, Accoto D, Trombetta M, Rainer A. Current trends in the design of scaffolds for computer-aided tissue engineering. Acta Biomater [Internet]. 2014 Feb;10(2):580–94. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24184176 DOI: https://doi.org/10.1016/j.actbio.2013.10.024
Brunello G, Sivolella S, Meneghello R, Ferroni L, Gardin C, Piattelli A, et al. Powder-based 3D printing for bone tissue engineering. Biotechnol Adv. 2016;34(5):740–53. DOI: https://doi.org/10.1016/j.biotechadv.2016.03.009
Park J, Lee SJ, Jung TG, Lee JH, Kim WD, Lee JY, et al. Surface modification of a three-dimensional polycaprolactone scaffold by polydopamine, biomineralization, and BMP-2 immobilization for potential bone tissue applications. Colloids Surfaces B Biointerfaces. 2021;199(September 2020):1–7. DOI: https://doi.org/10.1016/j.colsurfb.2020.111528
Ghasemi-Mobarakeh L, Kolahreez D, Ramakrishna S, Williams D. Key terminology in biomaterials and biocompatibility. Vol. 10, Current Opinion in Biomedical Engineering. Elsevier; 2019. p. 45–50. DOI: https://doi.org/10.1016/j.cobme.2019.02.004
Montoya C, Du Y, Gianforcaro AL, Orrego S, Yang M, Lelkes PI. On the road to smart biomaterials for bone research: definitions, concepts, advances, and outlook. Bone Res [Internet]. 2021 Feb 11 [cited 2022 May 18];9(1):1–16. Available from: https://www.nature.com/articles/s41413-020-00131-z DOI: https://doi.org/10.1038/s41413-020-00131-z
Wubneh A, Tsekoura EK, Ayranci C, Uludağ H. Current state of fabrication technologies and materials for bone tissue engineering. Acta Biomater. 2018 Oct 15;80:1–30. DOI: https://doi.org/10.1016/j.actbio.2018.09.031
Chocholata P, Kulda V, Babuska V. Fabrication of scaffolds for bone-tissue regeneration. Materials (Basel) [Internet]. 2019 Feb 14 [cited 2022 May 18];12(4):568. Available from: https://www.mdpi.com/1996-1944/12/4/568/htm DOI: https://doi.org/10.3390/ma12040568
Qu H, Fu H, Han Z, Sun Y. Biomaterials for bone tissue engineering scaffolds: A review [Internet]. Vol. 9, RSC Advances. Royal Society of Chemistry; 2019 [cited 2022 Sep 14]. p. 26252–62. Available from: https://pubs.rsc.org/en/content/articlehtml/2019/ra/c9ra05214c DOI: https://doi.org/10.1039/C9RA05214C
ISO/ASTM. Additive manufacturing — General principles — Fundamentals and vocabulary - ISO/ASTM52900-21 [Internet]. Book of Standards Volume: 10.04. 2021 [cited 2022 Sep 14]. Available from: https://www.astm.org/f3177-21.html
Germaini M, Belhabib S, Guessasma S, Deterre R, Corre P, Weiss P. Additive manufacturing of biomaterials for bone tissue engineering – A critical review of the state of the art and new concepts. Prog Mater Sci. 2022 Oct 1;130:100963. DOI: https://doi.org/10.1016/j.pmatsci.2022.100963
Garot C, Bettega G, Picart C. Additive Manufacturing of Material Scaffolds for Bone Regeneration: Toward Application in the Clinics. Adv Funct Mater [Internet]. 2021 Jan 1 [cited 2022 Aug 24];31(5):2006967. Available from: https://onlinelibrary.wiley.com/doi/full/10.1002/adfm.202006967 DOI: https://doi.org/10.1002/adfm.202006967
Cheah CM, Chua CK, Leong KF, Chua SW. Development of a Tissue Engineering Scaffold Structure Library for Rapid Prototyping. Part 1: Investigation and Classification. Int J Adv Manuf Technol [Internet]. 2003 Feb;21(4):291–301. Available from: http://link.springer.com/10.1007/s001700300034 DOI: https://doi.org/10.1007/s001700300034
Kafle A, Luis E, Silwal R, Pan HM, Shrestha PL, Bastola AK. 3d/4d printing of polymers: Fused deposition modelling (fdm), selective laser sintering (sls), and stereolithography (sla) [Internet]. Vol. 13, Polymers. Multidisciplinary Digital Publishing Institute; 2021 [cited 2022 Aug 24]. p. 3101. Available from: https://www.mdpi.com/2073-4360/13/18/3101/htm DOI: https://doi.org/10.3390/polym13183101
Moreno Madrid AP, Vrech SM, Sanchez MA, Rodriguez AP. Advances in additive manufacturing for bone tissue engineering scaffolds. Mater Sci Eng C. 2019 Jul 1;100:631–44. DOI: https://doi.org/10.1016/j.msec.2019.03.037
Chia HN, Wu BM. Recent advances in 3D printing of biomaterials. J Biol Eng [Internet]. 2015 Mar 1 [cited 2022 Aug 24];9(1):1–14. Available from: https://jbioleng.biomedcentral.com/articles/10.1186/s13036-015-0001-4 DOI: https://doi.org/10.1186/s13036-015-0001-4
Benedetti M, du Plessis A, Ritchie RO, Dallago M, Razavi SMJ, Berto F. Architected cellular materials: A review on their mechanical properties towards fatigue-tolerant design and fabrication. Vol. 144, Materials Science and Engineering R: Reports. Elsevier Ltd; 2021. p. 100606. DOI: https://doi.org/10.1016/j.mser.2021.100606
Dong G, Tang Y, Zhao YF. A survey of modeling of lattice structures fabricated by additive manufacturing. J Mech Des Trans ASME. 2017;139(10). DOI: https://doi.org/10.1115/1.4037305
Top N, Şahin İ, Gökçe H, Gökçe H. Computer-aided design and additive manufacturing of bone scaffolds for tissue engineering: state of the art. J Mater Res. 2021; DOI: https://doi.org/10.1557/s43578-021-00156-y
Bhate D, Penick CA, Ferry LA, Lee C. Classification and Selection of Cellular Materials in Mechanical Design: Engineering and Biomimetic Approaches. Designs [Internet]. 2019 Mar 19 [cited 2022 May 25];3(1):19. Available from: https://www.mdpi.com/2411-9660/3/1/19/htm DOI: https://doi.org/10.3390/designs3010019
Tang, Y., & Zhao YF. A survey of the design methods for additive manufacturing to improve functional performance. Rapid Prototyp J. 2016;22 Iss 3 p. DOI: https://doi.org/10.1108/RPJ-01-2015-0011
Chen H, Han Q, Wang C, Liu Y, Chen B, Wang J. Porous Scaffold Design for Additive Manufacturing in Orthopedics: A Review. Front Bioeng Biotechnol [Internet]. 2020 Jun 17 [cited 2022 May 6];8:609. Available from: www.frontiersin.org DOI: https://doi.org/10.3389/fbioe.2020.00609
Savio G, Rosso S, Meneghello R, Concheri G. Geometric modeling of cellular materials for additive manufacturing in biomedical field: A review. Appl Bionics Biomech. 2018;2018. DOI: https://doi.org/10.1155/2018/1654782
Zhou X, Feng Y, Zhang J, Shi Y, Wang L. Recent advances in additive manufacturing technology for bone tissue engineering scaffolds [Internet]. Vol. 108, International Journal of Advanced Manufacturing Technology. Springer; 2020 [cited 2022 May 6]. p. 3591–606. Available from: https://link.springer.com/article/10.1007/s00170-020-05444-1 DOI: https://doi.org/10.1007/s00170-020-05444-1
Kelly CN, Miller AT, Hollister SJ, Guldberg RE, Gall K. Design and Structure–Function Characterization of 3D Printed Synthetic Porous Biomaterials for Tissue Engineering [Internet]. Vol. 7, Advanced Healthcare Materials. John Wiley & Sons, Ltd; 2018 [cited 2022 May 6]. p. 1701095. Available from: https://onlinelibrary.wiley.com/doi/full/10.1002/adhm.201701095 DOI: https://doi.org/10.1002/adhm.201701095
Mohammadi H, Sepantafar M, Muhamad N, Bakar Sulong A. How Does Scaffold Porosity Conduct Bone Tissue Regeneration? Adv Eng Mater [Internet]. 2021 Oct 1 [cited 2022 May 6];23(10):2100463. Available from: https://onlinelibrary.wiley.com/doi/full/10.1002/adem.202100463 DOI: https://doi.org/10.1002/adem.202100463
Yang Y, Wang G, Liang H, Gao C, Peng S, Shen L, et al. Additive manufacturing of bone scaffolds. Int J Bioprinting [Internet]. 2019 [cited 2022 May 20];5(1). Available from: /pmc/articles/PMC7294697/ DOI: https://doi.org/10.18063/ijb.v5i1.148
Nsiempba KM, Wang M, Vlasea M. Geometrical degrees of freedom for cellular structures generation: A new classification paradigm [Internet]. Vol. 11, Applied Sciences (Switzerland). Multidisciplinary Digital Publishing Institute; 2021 [cited 2022 May 20]. p. 3845. Available from: https://www.mdpi.com/2076-3417/11/9/3845/htm DOI: https://doi.org/10.3390/app11093845
Chantarapanich N, Puttawibul P, Sucharitpwatskul S, Jeamwatthanachai P, Inglam S, Sitthiseripratip K. Scaffold library for tissue engineering: A geometric evaluation. Comput Math Methods Med. 2012;2012. DOI: https://doi.org/10.1155/2012/407805
Babaie E, Bhaduri SB. Fabrication Aspects of Porous Biomaterials in Orthopedic Applications: A Review [Internet]. Vol. 4, ACS Biomaterials Science and Engineering. American Chemical Society; 2018 [cited 2022 May 6]. p. 1–39. Available from: https://pubs.acs.org/doi/abs/10.1021/acsbiomaterials.7b00615 DOI: https://doi.org/10.1021/acsbiomaterials.7b00615
Cubo-Mateo N, Rodríguez-Lorenzo LM. Design of thermoplastic 3D-Printed scaffolds for bone tissue engineering: Influence of parameters of “hidden” importance in the physical properties of scaffolds. Polymers (Basel) [Internet]. 2020 Jul 13 [cited 2022 Oct 6];12(7):1–14. Available from: https://www.mdpi.com/2073-4360/12/7/1546/htm DOI: https://doi.org/10.3390/polym12071546
Boccaccio A, Uva AE, Fiorentino M, Mori G, Monno G. Geometry Design Optimization of Functionally Graded Scaffolds for Bone Tissue Engineering: A Mechanobiological Approach. PLoS One [Internet]. 2016;11(1):e0146935. Available from: http://dx.plos.org/10.1371/journal.pone.0146935 DOI: https://doi.org/10.1371/journal.pone.0146935
Deng F, Liu L, Li Z, Liu J. 3D printed Ti6Al4V bone scaffolds with different pore structure effects on bone ingrowth. J Biol Eng [Internet]. 2021;15(1):1–13. Available from: https://doi.org/10.1186/s13036-021-00255-8 DOI: https://doi.org/10.1186/s13036-021-00255-8
Liu F, Ran Q, Zhao M, Zhang T, Zhang DZ, Su Z. Additively manufactured continuous cell-size gradient porous scaffolds: Pore characteristics, mechanical properties and biological responses in vitro. Materials (Basel). 2020;13(11). DOI: https://doi.org/10.3390/ma13112589
Ataee A, Li Y, Fraser D, Song G, Wen C. Anisotropic Ti-6Al-4V gyroid scaffolds manufactured by electron beam melting (EBM) for bone implant applications. Mater Des. 2018 Jan 5;137:345–54. DOI: https://doi.org/10.1016/j.matdes.2017.10.040
Pattnaik A, Sanket AS, Pradhan S, Sahoo R, Das S, Pany S, et al. Designing of gradient scaffolds and their applications in tissue regeneration. Biomaterials. 2023 May 1;296:122078. DOI: https://doi.org/10.1016/j.biomaterials.2023.122078
Lee SS, Du X, Kim I, Ferguson SJ. Scaffolds for bone-tissue engineering. Matter. 2022 Sep 7;5(9):2722–59. DOI: https://doi.org/10.1016/j.matt.2022.06.003
Wang X, Xu S, Zhou S, Xu W, Leary M, Choong P, et al. Topological design and additive manufacturing of porous metals for bone scaffolds and orthopaedic implants: A review. Vol. 83, Biomaterials. 2016. p. 127–41. DOI: https://doi.org/10.1016/j.biomaterials.2016.01.012
Hössinger-Kalteis A, Reiter M, Jerabek M, Major Z. Overview and comparison of modelling methods for foams. J Cell Plast. 2020; DOI: https://doi.org/10.1177/0021955X20966329
Bhate D. Four questions in cellular material design. Materials (Basel). 2019;12(7). DOI: https://doi.org/10.3390/ma12071060
du Plessis A, Broeckhoven C, Yadroitsava I, Yadroitsev I, Hands CH, Kunju R, et al. Beautiful and Functional: A Review of Biomimetic Design in Additive Manufacturing. Addit Manuf [Internet]. 2019 May 1 [cited 2022 May 27];27(March):408–27. Available from: https://doi.org/10.1016/j.addma.2019.03.033 DOI: https://doi.org/10.1016/j.addma.2019.03.033
Hargroves K, Smith M. Innovation inspired by nature: Biomimicry. Ecos Sci Sustain. 2006;(129):27–9.
Caetano I, Santos L, Leitão A. Computational design in architecture: Defining parametric, generative, and algorithmic design. Front Archit Res. 2020 Jun 1;9(2):287–300. DOI: https://doi.org/10.1016/j.foar.2019.12.008
Frayssinet E, Colabella L, Cisilino AP. Design and assessment of the biomimetic capabilities of a Voronoi-based cancellous microstructure. J Mech Behav Biomed Mater. 2022 Jun 1;130:105186. DOI: https://doi.org/10.1016/j.jmbbm.2022.105186
Du Y, Liang H, Xie D, Mao N, Zhao J, Tian Z, et al. Design and statistical analysis of irregular porous scaffolds for orthopedic reconstruction based on voronoi tessellation and fabricated via selective laser melting (SLM). Mater Chem Phys. 2020;239(July 2019):1–9. DOI: https://doi.org/10.1016/j.matchemphys.2019.121968
Zhu J, Zhao H, Wang C, Zhou L, Yuan S, Zhang W. A review of topology optimization for additive manufacturing: Status and challenges. Chinese J Aeronaut [Internet]. 2021;34(1):91–110. Available from: https://www.sciencedirect.com/science/article/pii/S1000936120304520 DOI: https://doi.org/10.1016/j.cja.2020.09.020
Wu J, Zhang Y, Lyu Y, Cheng L. On the Various Numerical Techniques for the Optimization of Bone Scaffold [Internet]. Vol. 16, Materials. Multidisciplinary Digital Publishing Institute; 2023 [cited 2023 Jul 20]. p. 974. Available from: https://www.mdpi.com/1996-1944/16/3/974/htm DOI: https://doi.org/10.3390/ma16030974
Wu N, Li S, Zhang B, Wang C, Chen B, Han Q, et al. The advances of topology optimization techniques in orthopedic implants: A review. Med Biol Eng Comput [Internet]. 2021;59(9):1673–89. Available from: https://doi.org/10.1007/s11517-021-02361-7 DOI: https://doi.org/10.1007/s11517-021-02361-7
Pires T, Dunlop JWC, Fernandes PR, Castro APG. Challenges in computational fluid dynamics applications for bone tissue engineering. Proc R Soc A [Internet]. 2022 [cited 2022 May 5];478(2257). Available from: https://royalsocietypublishing.org/doi/full/10.1098/rspa.2021.0607
Zhang S, Li X, Qi Y, Ma X, Qiao S, Cai HX, et al. Comparison of Autogenous Tooth Materials and Other Bone Grafts [Internet]. Vol. 18, Tissue Engineering and Regenerative Medicine. Springer; 2021 [cited 2022 Jun 3]. p. 327–41. Available from: https://link.springer.com/article/10.1007/s13770-021-00333-4 DOI: https://doi.org/10.1007/s13770-021-00333-4
Yan Y, Chen H, Zhang H, Guo C, Yang K, Chen K, et al. Vascularized 3D printed scaffolds for promoting bone regeneration. Biomaterials. 2019;190–191(August 2018):97–110. DOI: https://doi.org/10.1016/j.biomaterials.2018.10.033
Aoki K, Saito N. Biodegradable Polymers as Drug Delivery Systems for Bone Regeneration. Pharm 2020, Vol 12, Page 95 [Internet]. 2020 Jan 24 [cited 2022 Jun 3];12(2):95. Available from: https://www.mdpi.com/1999-4923/12/2/95/htm DOI: https://doi.org/10.3390/pharmaceutics12020095
Torgbo S, Sukyai P. Bacterial cellulose-based scaffold materials for bone tissue engineering. Appl Mater Today. 2018;11:34–49. DOI: https://doi.org/10.1016/j.apmt.2018.01.004
Karageorgiou V, Kaplan D. Porosity of 3D biomaterial scaffolds and osteogenesis. Biomaterials [Internet]. 2005;26:5474–91. Available from: http://www.sciencedirect.com/science/article/pii/S0142961205001511 DOI: https://doi.org/10.1016/j.biomaterials.2005.02.002
Deb P, Deoghare AB, Borah A, Barua E, Das Lala S. Scaffold Development Using Biomaterials: A Review. Mater Today Proc. 2018;5(5):12909–19. DOI: https://doi.org/10.1016/j.matpr.2018.02.276
Nikolova MP, Chavali MS. Recent advances in biomaterials for 3D scaffolds: A review. Bioact Mater. 2019;4(October 2019):271–92. DOI: https://doi.org/10.1016/j.bioactmat.2019.10.005
Zhang S, Vijayavenkataraman S, Lu WF, Fuh JYHH. A review on the use of computational methods to characterize, design, and optimize tissue engineering scaffolds, with a potential in 3D printing fabrication. J Biomed Mater Res - Part B Appl Biomater [Internet]. 2019 Jul 1 [cited 2022 May 4];107(5):1329–51. Available from: https://onlinelibrary.wiley.com/doi/full/10.1002/jbm.b.34226 DOI: https://doi.org/10.1002/jbm.b.34226
Knychala J, Bouropoulos N, Catt CJ, Katsamenis OL, Please CP, Sengers BG. Pore geometry regulates early stage human bone marrow cell tissue formation and organisation. Ann Biomed Eng [Internet]. 2013 Feb 13 [cited 2022 May 6];41(5):917–30. Available from: https://link.springer.com/article/10.1007/s10439-013-0748-z DOI: https://doi.org/10.1007/s10439-013-0748-z
Li L, Li Y, Yang L, Yu F, Zhang K, Jin J, et al. Polydopamine coating promotes early osteogenesis in 3D printing porous Ti6Al4V scaffolds. Ann Transl Med [Internet]. 2019 Jun [cited 2022 May 6];7(11):240–240. Available from: https://atm.amegroups.com/article/view/25688/html DOI: https://doi.org/10.21037/atm.2019.04.79
Xia P, Luo Y. Vascularization in tissue engineering: The architecture cues of pores in scaffolds. J Biomed Mater Res Part B Appl Biomater [Internet]. 2022 May 1 [cited 2022 May 6];110(5):1206–14. Available from: https://onlinelibrary.wiley.com/doi/full/10.1002/jbm.b.34979 DOI: https://doi.org/10.1002/jbm.b.34979
Velasco MA, Lancheros Y, Garzón-Alvarado DA. Geometric and mechanical properties evaluation of scaffolds for bone tissue applications designing by a reaction-diffusion models and manufactured with a material jetting system. J Comput Des Eng [Internet]. 2016;3:385–97. Available from: www.sciencedirect.com DOI: https://doi.org/10.1016/j.jcde.2016.06.006
Alonzo M, Alvarez Primo F, Anil Kumar S, Mudloff JA, Dominguez E, Fregoso G, et al. Bone tissue engineering techniques, advances, and scaffolds for treatment of bone defects. Curr Opin Biomed Eng. 2021;17(September 2020). DOI: https://doi.org/10.1016/j.cobme.2020.100248
Prasad A. State of art review on bioabsorbable polymeric scaffolds for bone tissue engineering. In: Materials Today: Proceedings. Elsevier; 2021. p. 1391–400. DOI: https://doi.org/10.1016/j.matpr.2020.11.622
Lv Y, Wang B, Liu G, Tang Y, Lu E, Xie K, et al. Metal Material, Properties and Design Methods of Porous Biomedical Scaffolds for Additive Manufacturing: A Review. Front Bioeng Biotechnol. 2021;9(March):1–16. DOI: https://doi.org/10.3389/fbioe.2021.641130
Roseti L, Parisi V, Petretta M, Cavallo C, Desando G, Bartolotti I, et al. Scaffolds for Bone Tissue Engineering: State of the art and new perspectives. Mater Sci Eng C. 2017;78:1246–62. DOI: https://doi.org/10.1016/j.msec.2017.05.017
Liu H, Ahlinder A, Yassin MA, Finne-Wistrand A, Gasser TC. Computational and experimental characterization of 3D-printed PCL structures toward the design of soft biological tissue scaffolds. Mater Des. 2020;188:108488. DOI: https://doi.org/10.1016/j.matdes.2020.108488
Öhman-Mägi C, Holub O, Wu D, Hall RM, Persson C. Density and mechanical properties of vertebral trabecular bone—A review. JOR Spine [Internet]. 2021 Dec 1 [cited 2023 Jun 14];4(4):e1176. Available from: https://onlinelibrary.wiley.com/doi/full/10.1002/jsp2.1176 DOI: https://doi.org/10.1002/jsp2.1176
Collins MN, Ren G, Young K, Pina S, Reis RL, Oliveira JM. Scaffold Fabrication Technologies and Structure/Function Properties in Bone Tissue Engineering. Adv Funct Mater [Internet]. 2021 May 1 [cited 2022 May 4];31(21):2010609. Available from: https://onlinelibrary.wiley.com/doi/full/10.1002/adfm.202010609 DOI: https://doi.org/10.1002/adfm.202010609
Zerankeshi M, Bakhshi R, Alizadeh R. Polymer/metal composite 3D porous bone tissue engineering scaffolds fabricated by additive manufacturing techniques: A review. Vol. 25, Bioprinting. Elsevier; 2022. p. e00191. DOI: https://doi.org/10.1016/j.bprint.2022.e00191
Gajewski T, Krzysztof Grabski J, Somnic J, Jo BW. Status and Challenges in Homogenization Methods for Lattice Materials. Mater 2022, Vol 15, Page 605 [Internet]. 2022 Jan 14 [cited 2022 Aug 24];15(2):605. Available from: https://www.mdpi.com/1996-1944/15/2/605/htm
Turnbull G, Clarke J, Picard F, Riches P, Jia L, Han F, et al. 3D bioactive composite scaffolds for bone tissue engineering. Vol. 3, Bioactive Materials. Elsevier; 2018. p. 278–314. DOI: https://doi.org/10.1016/j.bioactmat.2017.10.001
Pires T, Dunlop JWC, Fernandes PR, Castro APG. Challenges in computational fluid dynamics applications for bone tissue engineering [Internet]. Proceedings of the Royal Society A: Mathematical, Physical and Engineering Sciences The Royal Society; 2022 p. 1–20. Available from: https://royalsocietypublishing.org/doi/full/10.1098/rspa.2021.0607 DOI: https://doi.org/10.1098/rspa.2021.0607
Zhang K, Fan Y, Dunne N, Li X. Effect of microporosity on scaffolds for bone tissue engineering [Internet]. Vol. 5, Regenerative Biomaterials. Oxford Academic; 2018 [cited 2022 May 6]. p. 115–24. Available from: https://academic.oup.com/rb/article/5/2/115/4838883 DOI: https://doi.org/10.1093/rb/rby001
Prakoso AT, Basri H, Adanta D, Yani I, Ammarullah MI, Akbar I, et al. The Effect of Tortuosity on Permeability of Porous Scaffold. Biomedicines. 2023;11(2):1–17. DOI: https://doi.org/10.3390/biomedicines11020427
Downloads

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-CompartirIgual 4.0.
Los autores que publican en esta revista están de acuerdo con los siguientes términos:
Los autores ceden los derechos patrimoniales a la revista y a la Universidad del Valle sobre los manuscritos aceptados, pero podrán hacer los reusos que consideren pertinentes por motivos profesionales, educativos, académicos o científicos, de acuerdo con los términos de la licencia que otorga la revista a todos sus artículos.
Los artículos serán publicados bajo la licencia Creative Commons 4.0 BY-NC-SA (de atribución, no comercial, sin obras derivadas).

 https://orcid.org/0000-0003-4436-9443
https://orcid.org/0000-0003-4436-9443 https://orcid.org/0000-0002-0979-3241
https://orcid.org/0000-0002-0979-3241 https://orcid.org/0000-0003-0072-3738
https://orcid.org/0000-0003-0072-3738